Deep Venous Thrombosis
The Interventional Radiologists at MRA specialize in the broad spectrum of venous diseases, including varicose veins, superficial venous insufficiency, deep venous thrombosis, May-Thurner syndrome, post-thrombotic syndrome, and lower extremity swelling.
What is Deep Venous Thrombosis?
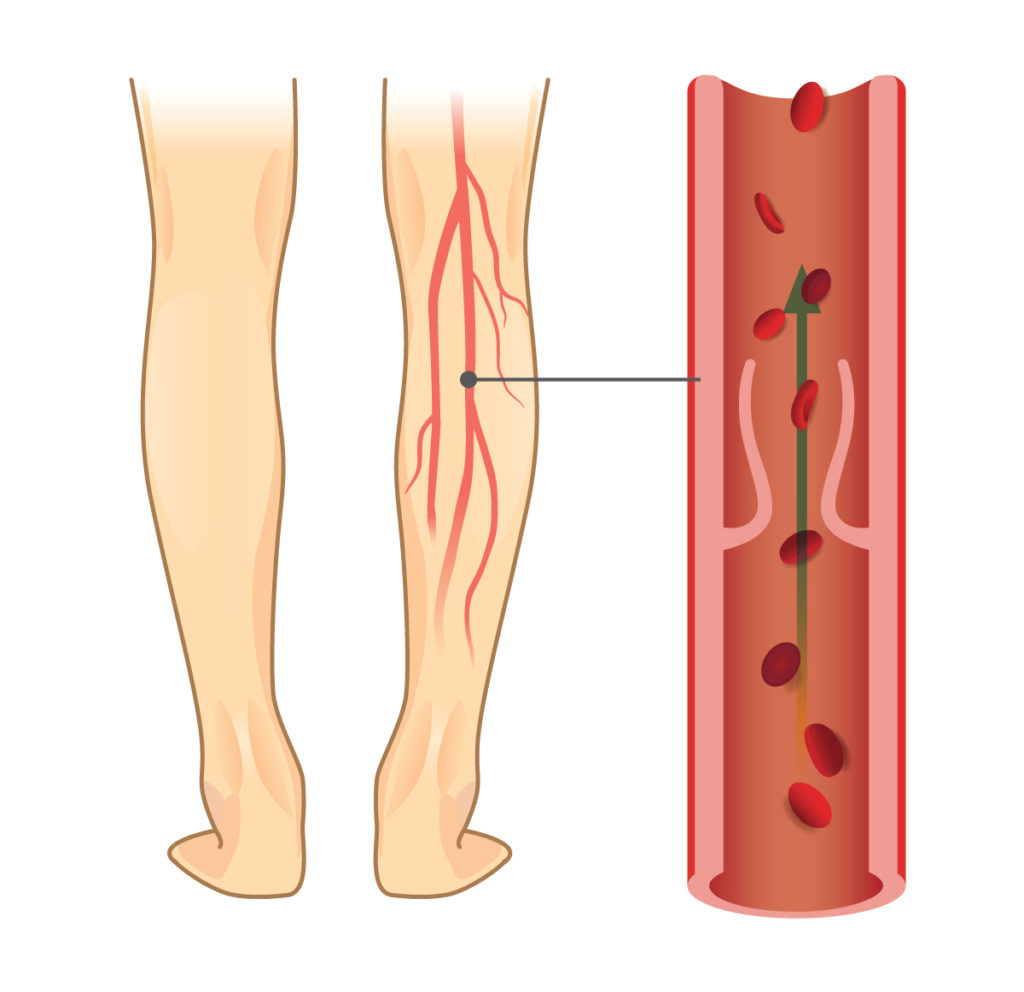
Deep venous thrombosis (DVT) is a condition in which a blood clot forms within a vein. Normally, blood flows freely through the veins to return to the heart. When a vein is blocked by a blood clot, it can produce swelling, pain, and redness in the affected part of the body. While DVT can occur anywhere in the body, the most common site is the leg.
If part of the clot breaks off, it can travel through the veins to other parts of the body. When the clot travels to the lungs, it is called a pulmonary embolism. This is a serious condition which can compromise the function of the lungs and heart.
Typically, your health care provider will first assess your symptoms and perform a physical exam. If these suggest that DVT is possible, an ultrasound will be performed which usually makes the diagnosis. Sometimes a CT scan is also performed if there is concern for clot extending into the veins of the pelvis, or if there is concern for pulmonary embolism. Our doctors are highly trained in the interpretation of imaging for DVT.
DVT is typically treated with blood thinning medications. For most patients, this is sufficient, and the clot slowly dissolves with time.
Some patients cannot be safely treated with blood thinners (for example if they have a history of significant bleeding or recent major surgery). In those patients, a protective device called an IVC Filter can be inserted into the largest vein in the abdomen, the Inferior Vena Cava (IVC).
In a small percentage of patients, the clot does not improve with blood thinners alone. This is most common when there is a large amount of clot, or the clot extends into the veins of the pelvis. In those cases, a minimally invasive procedure called Catheter Directed Therapy may be required to help eliminate the clot.
The Interventional Radiologists at MRA are well versed in the full spectrum of treatment for DVT. Each case of DVT is unique and requires a plan to manage the initial episode as well as prevent future episodes.
All of the procedures below are performed through an incision in the skin the size of a pencil tip. A catheter (thin, flexible tube) is inserted directly into the vein, and navigated to the appropriate area using advanced imaging guidance.
Catheter Directed Therapy – When DVT symptoms are severe and/or not improving with blood thinners alone, this minimally-invasive procedure can be performed to help dissolve the clot (thrombolysis) or physically remove it (thrombectomy).
Angioplasty/Stenting – If there is a narrowing or blockage in the veins of the abdomen, pelvis, or legs which has caused the clot to form, this can often be treated. This may require angioplasty (stretching of the vein using a balloon) or stenting (placement of a metal mesh tube to keep the vein open).
IVC filter placement – When patients with DVT cannot safely be treated with blood thinners, an IVC filter can be inserted into the largest vein in the abdomen, the Inferior Vena Cava (IVC). This device looks like an upside-down umbrella, and serves to trap any clot which breaks off from the legs and travels towards the heart and lungs.
IVC filter removal – If a patient no longer requires their IVC filter (if the clot has resolved and they are no longer at risk), it should be removed if possible. The specialists at MRA have experience in a wide range of techniques to remove filters, with a success rate near 100%.
May-Thurner syndrome results from an abnormal compression of the left common iliac vein (in the pelvis), by an adjacent artery. It can result in DVT of the left leg, because blood cannot easily pass this site of blockage. When patients with May-Thurner Syndrome develop DVT, it is an important entity to recognize, because it will often require definitive treatment (usually stenting) to prevent future episodes of clotting. Additionally, failure to address the blockage can lead to long term damage to the leg veins (post-thrombotic syndrome).
Post-thrombotic syndrome, or chronic venous insufficiency, results when veins of the pelvis and legs become damaged following DVT. The pressure in the veins increases, and results in symptoms including chronic leg swelling, a sensation of leg heaviness/fatigue, discoloration of the skin, and/or leg ulcers. This is most commonly seen in patients that suffered from a large burden of clot, or those who have abnormal blockages of the veins (for example in May-Thurner Syndrome, or iliac vein/IVC occlusions). Preventing post-thrombotic syndrome is an important goal in the initial therapy of DVT. For those patients that go on to develop post-thrombotic syndrome, our interventional radiologists are well versed in the medical and procedural treatment of this disease.
The DVT treatments above are typically covered by insurance. Your out-of-pocket expense will depend on your specific insurance plan.
Request a consultation today:
One of our expert Interventional Radiologists will personally review your imaging and case with you and help develop a treatment plan that is right for you.
Patients, please note that services may require a referral from your primary care or another provider, but we can help facilitate that process if treatment is deemed necessary. Telehealth consultations may be available depending on the type of procedure required.